How to determine the degree of chronic venous insufficiency. Venous insufficiency
Chronic venous insufficiency of the lower extremities is observed in 25% of the total population. In most cases, the disease occurs in residents of eastern countries. The reason is a sedentary lifestyle and work that requires constant sitting or standing. Chronic lower extremity pain (pathogenesis) occurs due to poor blood circulation. The vertical position of the body is a condition that is not characteristic of any mammal on earth. The lower limbs always have poor blood circulation due to gravity.
Features of the circulatory system
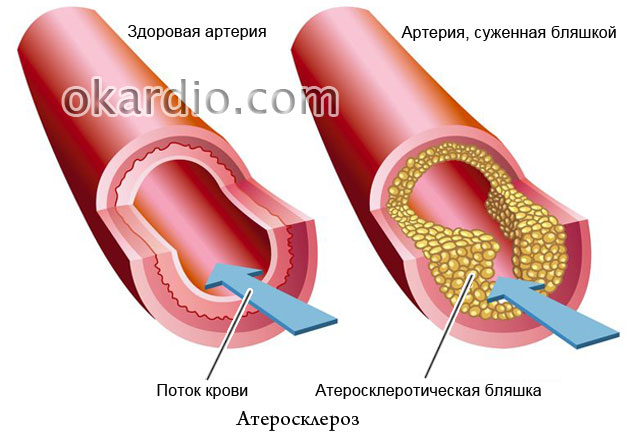
Blood passes through the largest vessels - arteries, which have branches into small vessels - arterioles and capillaries. The movement of blood through small blood vessels does not have any difficulty because the blood flows at high pressure.
Through the venous system, blood does not reach the lower extremities in full, since it is affected by the force of gravity. The movement of blood through the veins is ensured by valves, the main function of which is to close and open. When the valve is closed, blood moves upward. This happens due to the contractile function of the muscular system of the legs. When the walls of the blood vessels lose their elasticity and begin to stretch, the valve stops functioning correctly. The situation is aggravated by blockage of blood vessels with blood clots and cholesterol plaques.
Chronic venous insufficiency of the legs is provoked due to any circulatory disorders. A complete cure for venous insufficiency is not possible.
Chronic venous insufficiency of the lower extremities can be congenital or acquired due to leg injuries or blockage of the veins. The disease is a violation of the circulatory process in the legs, when blood, moving from bottom to top, cannot completely pass through the veins and stagnates in them, causing dilation of the blood vessels. Blood presses on the walls of blood vessels, causing them to weaken and expand.
The symptoms of the disease and the causes of its occurrence depend on the type of blood flow disorder.
Chronic venous insufficiency of the lower extremities:
- Zero stage– the onset of a disease in which damaged vein walls are not detected upon examination. The main symptom is the appearance of a vascular venous network, which does not cause pain or discomfort.
- Stagnant processes of 1st degree of venous insufficiency- in the evening, after a day of work, the lower limbs swell. This is expressed in the fact that a person has traces of the elastic bands of his socks and the seams of his trousers. There is no swelling of the toes. There is a feeling of heaviness in the lower extremities. Most patients do not pay attention to these signs, delaying treatment and aggravating the condition.
- Signs of 2nd degree– pain in the lower extremities, feeling of fullness. The pain intensifies at night. Swelling is observed both in the evening and in the morning. Swollen veins appear through the skin and cause pain upon palpation. At this stage of the development of the disease, patients, unfortunately, are in no hurry to see a doctor, trying to use traditional medicine methods, which in some cases gives positive dynamics.
- 3rd degree– constant swelling of the lower extremities, the skin is pale and cold. The pain syndrome is pronounced. In many cases, convulsive muscle contractions begin.
- 4th degree– disruption of the blood circulation process has a negative effect on the skin. Brown spots begin to appear on the legs, and inflammatory lesions appear. Some patients develop eczema - the skin at the site of damaged veins becomes too thin and peeling appears. At this stage of the disease, a person requires emergency medical care.
- Symptoms of the fifth,very severe Chronic leg insufficiency is characterized by formation. The skin begins to thicken and becomes very pale. At this stage, the vein may begin to become clogged with blood clots.
- Sixth, extremely severe stage of chronic venous insufficiency of the lower extremities- has the following symptoms - the ulcers do not heal on their own, they constantly expand. If blood clots form, the disease can only be cured through surgery.

Causes
Most people on the planet have a genetic predisposition to the disease. In some cases, the development of the disease is associated with age-related changes, since the walls of the veins become less elastic over time, stretch, and the venous valve is not able to ensure tight closure of the lumen.
The main factors that can cause the development of venous circulation insufficiency in the lower extremities:
- Regular intake of medications containing hormones.
- Pregnancy and labor. During the period of bearing a child, the lower limbs and pelvic organs experience excessive stress. The expanding uterus and the increasing weight of the fetus puts pressure on the veins in the pelvis, leading to their compression and provoking stagnant processes.
- Sedentary lifestyle. In people who have a “sedentary” job and do not bother themselves with physical activity, a venous network appears over time, which provokes the development of more serious pathological processes in the circulatory system.
- A position of the body in a lying or sitting position that lasts for hours. In some cases, the patient is recommended to change the nature of his work activity in order to recover from the disease.
- Excess body weight.
- Lifting heavy loads, which is associated with professional activities, is observed among athletes - weightlifters.
- Frequent visits to the steam room, taking hot baths.
As medical practice shows, most patients diagnosed with chronic venous insufficiency seek medical help only in cases where the disease has caused a number of severe complications, and the treatment will be very complex and long.
Treatment methods include drug and surgical treatment of venous insufficiency, depending on the stage of the disease. Each patient undergoing treatment needs to change their daily routine to include several hours of physical activity. If you are overweight, you need to lose weight.
The first two stages of the disease do not require serious treatment. As a rule, the patient is prescribed medications that increase the tone of the walls of blood vessels - Ginkor-Fort, Detralex. A method is used in which a drug is administered that stops the process of blood outflow in the damaged vein in order to narrow it.

The second – fourth stage is treated with antihistamines. If there is a high risk of complications, medications that have an anti-inflammatory effect are prescribed. The choice of medications depends on the individual characteristics of the patient and is prescribed only by the attending physician.
The most severe stages of the disease are 5 and 6, during which ulcers form, and medications with a general and local spectrum of action are prescribed. It is mandatory to treat ulcers daily with decoctions of chamomile and other remedies that have a soothing and disinfecting effect.
Surgical operations are performed only in the last stages of the disease, in the absence of positive dynamics from taking medications. The main types of operations are phlebectomy: removal of the damaged part of the vessel and bypass surgery - complete removal of the vein, and creation of a bypass to ensure blood flow.
Use is only possible to relieve symptoms. For example, to relieve swelling and pain, it is recommended to apply cold compresses to the lower extremities daily.
To normalize the composition of the blood and reduce its viscosity to prevent the formation of blood clots, you can use the following recipe - hops or sweet clover herb in the form of a decoction. Take one glass before meals.
Horse chestnut has a beneficial effect on veins and blood. To prepare the decoction, you need to pour a tablespoon of the ingredient into one glass of boiling water.

Prevention
Measures to prevent the development of complications:
- Wearing comfortable shoes. Shoes with stiletto heels are excluded.
- Regular rest for the lower extremities, during which the feet should be higher than the level of the head.
- Playing sports. Preference is given to active activities - running, cycling, swimming, dancing, aerobics.
- Wearing compression stockings and socks.
- Cold and hot shower. Alternating exposure of the skin to cold and hot water causes the veins to contract, which helps maintain the elasticity of their walls.
To prevent the occurrence of venous disease of the legs, it is necessary to lead an active lifestyle and take preventive measures to prevent the development of varicose veins.
Venous insufficiency is a condition in which the veins cannot transport blood from the extremities to the heart in sufficient quantities. Venous insufficiency of the lower extremities - its symptoms are familiar to men and women, and treatment causes difficulties even for specialists.

The most common symptom is a dull pain in the legs that becomes unbearable by the end of the day. The pain intensifies after prolonged standing. The symptoms are caused by stagnation of venous blood in the legs, which leads to swelling. This causes swelling, tingling and even cramps.
The skin becomes pale and then reddens and looks brownish-red. In the ankles, the limb increases in volume, and itching occurs. If venous insufficiency is associated with dilated veins, then they become noticeable as they turn blue and become bulging.
Then trophic disorders progress, the skin looks scaly and becomes covered with ulcers. The patient is accompanied by heaviness of the legs and noticeable swelling.
Venous insufficiency develops in the absence of proper blood circulation in the extremities. Circulation does not occur because blood flow is blocked by a blocked vein or valve insufficiency. As a result, blood begins to collect in the lower extremities. The venous valve apparatus serves to direct blood flow in the right direction (to the heart). If the valves are damaged, some of the blood remains in the lower extremities. Other reasons:
- Formation of blood clots in deep veins;
- Varicose veins of superficial veins;
- Blood clots that obstruct blood flow;
- Age over 50;
- Fluctuations in progesterone associated with pregnancy;
- Excess weight;
- Sedentary work;
- Muscle weakness;
- Oncological diseases;
- Injuries;
- Genetic abnormalities;
- Smoking.
Venous insufficiency is diagnosed by a doctor during a visual examination. An additional method is the use of Doppler ultrasound. The examination shows valve defects, blood clots, size and shape of the vessel. To clarify the diagnosis, MRI or tomography is used.

Treatment of venous insufficiency of the lower extremities
The most worrying symptoms are pain and swelling. Therefore, treatment primarily consists of relieving these symptoms.
Drug treatment - taking blood thinners. Anticoagulants dissolve blood clots and restore vessel patency. The drugs also prevent the formation of blood clots.
Medicines for the treatment of venous insufficiency:
- Avenue - the drug increases the tone of the vascular wall, increases lymphatic outflow, reduces fragility and capillary permeability.
- Detralex – protects the vascular wall from damage, tones the veins.
- Aescusan is a drug made from horse chestnut. Increases the production of catecholamines, protects veins from damage, increases the elasticity of the vascular wall.
- Venarus – improves circulation and venous outflow.
- Phlebodia – promotes venous blood flow, reduces swelling of the legs.
Laminin, bilobil, normoven have a similar effect.
Compression clothing - the mechanism of action is due to mechanical pressure on the vessels, which pushes blood in the right direction. They are in the pharmacy and are available to everyone. They differ in size, color and material. Compression stockings are characterized by a compression gradient.
Medical dressings for the treatment of trophic ulcers - use antiseptics, ointments, and folk remedies. To treat the acute stage, cold compresses are used - a chilled gauze swab is applied to the affected area for two minutes, then cooled again in a container with ice. The procedure is carried out for 40 minutes.
Non-surgical treatments
Endovenous thermal ablation is an effective and painless procedure for treating venous insufficiency. It is performed using a laser and high-frequency radio waves. This prevents the progression of the disease.
 The method involves injecting a sclerosing solution into the vein, which fills the dilation and causes the vessel to stick together. This eliminates pain and swelling. The drug is eliminated from the body on its own. In the early stages, the technique gives positive results no worse than after surgery. In more advanced cases, combined treatment is necessary: surgery, medication and physical therapy.
The method involves injecting a sclerosing solution into the vein, which fills the dilation and causes the vessel to stick together. This eliminates pain and swelling. The drug is eliminated from the body on its own. In the early stages, the technique gives positive results no worse than after surgery. In more advanced cases, combined treatment is necessary: surgery, medication and physical therapy.
Benefits of sclerotherapy:
- No scars are left;
- The integrity of the vein is preserved;
- Well tolerated psychologically;
- Convenient to use for chronic varicose veins;
- Can be prescribed in combination with other treatment methods.
Surgical treatment of venous insufficiency: venous bypass - eliminating the problem by transplanting a healthy section of the vessel.
Ligation and purification
 The surgical procedure consists of stitching the affected area and clearing the varicose veins. Loops (ligatures) are placed through the skin using a special tool, and the sutures are tied from the outside. After contraction of the vessel, the thrombus is removed. The disadvantage of this method is that relapse is possible.
The surgical procedure consists of stitching the affected area and clearing the varicose veins. Loops (ligatures) are placed through the skin using a special tool, and the sutures are tied from the outside. After contraction of the vessel, the thrombus is removed. The disadvantage of this method is that relapse is possible.
Phlebectomy – removal of blood clots and the affected area of the vein. Microinvasive intervention is performed through the skin on an outpatient basis. Modern methods: laser phlebectomy and radiofrequency obliteration.
Chronic venous insufficiency of the lower extremities
Long-term disruption of the venous outflow of blood and the development of venous obstruction leads to chronic venous insufficiency. Pathogenesis is associated with the destruction of valves by thrombosis, phlebitis, injuries and burns. The weakening of muscle strength, which is necessary to create sufficient blood pressure, is not the direct cause of chronic venous insufficiency, but contributes to the exacerbation of the disease.
Chronic venous insufficiency: clinical models
Symptoms of chronic venous insufficiency are grouped into the most common clinical variants:
- Uncomplicated venous varicose veins;
- Superficial thrombophlebitis;
- Varicose veins are generalized vascular lesions combined with pain, swelling and skin changes. Often the cause is pathology of the superficial veins, treatment of which will help correct the situation;
- Venous hypertension syndrome – pain in the legs when standing. The pain goes away in a sitting position. Sometimes this is the only sign. The patients are young women. The cause is deep vein obstruction; surgical treatment relieves pain.
- Swelling of the extremities - occurs in older people who lead a sedentary lifestyle. More common in women.
- A complex of multisystem venous pathologies - a disorder in the system of superficial, deep and perforated veins.
Chronic venous insufficiency is diagnosed using anamnestic data and an external objective examination. Duplex ultrasound allows you to establish the stage of the disease and confirm or deny the presence of venous thrombosis. Other methods: venography, CT, MR angiography.
Minor vein injuries may cause no symptoms. On the other hand, the pathology of the deep veins, as well as the combination with a violation of the outflow from the superficial ones, leads to serious consequences. Another factor that causes peeling, impaired capillary circulation, lymph stagnation and decreased sensitivity is high blood pressure. Symptoms of chronic venous insufficiency are as follows:

Trophic venous ulcers are difficult to cure; they progress and recur. Risk factors for exacerbation of venous ulcers:
- Postthrombotic symptom;
- Blockage in the iliofemoral system;
- Deep vein insufficiency;
- Resistant venous hypertension.
The development of chronic failure depends on the rate of disease progression.
Chronic venous insufficiency: prevention
An active lifestyle and physical exercises aimed at strengthening the muscles of the lower leg are an excellent way to prevent venous insufficiency. Physical activity should not be only static, it should be alternated with dynamic (running, swimming). Walking for 40 minutes every day will strengthen the muscles and vein wall.
When lying down, your legs should be kept elevated. It must be taken into account that excess weight increases the load on the venous system and complicates the outflow from the limbs. High heels also prevent the venous system from moving blood freely in the vessels.
The use of oral contraceptives is a risk of developing venous insufficiency. In this case, you should regularly (twice a year) undergo ultrasound examination of the blood vessels of the legs. The same measures should be taken by pregnant women. If necessary, compression stockings should be used.
Quite a large number of people have encountered a disease such as venous insufficiency. The first symptoms of the disease are a feeling of heaviness in the legs, rapid fatigue when walking, and the appearance of a bright network of venous capillaries on the skin of the extremities. If you do not pay due attention to such changes, you risk venous insufficiency degree 2.
Causes of the disease
As a rule, the causes of the disease are:
. age-related changes occurring in our body;Hormonal changes;
Sedentary lifestyle;
Overweight;
Individual predisposition to decreased tone of the walls of venous vessels.
The second stage of venous insufficiency is characterized by hyperpigmentation, which is a darkening of the skin. This phenomenon is caused by the accumulation of hemosiderin in the epidermis, a specific pigment that colors the skin dark. At the same time, the patient may experience so-called indurative subcutaneous cellulite. The legs of patients suffering from stage 2 venous insufficiency may swell.
The cause of all the above ailments is a violation of tissue trophism in the lower extremities, associated with stagnation of blood and lymph. Our medical center is ready to offer you a whole range of medical services aimed at combating venous insufficiency and its manifestations, both in the early stages of the disease and and at its later stages.
Our medical institution is staffed by specialists with extensive experience. The leading phlebologists and angiosurgeons of the center have in their track record more than one successfully performed operation and timely prescribed medication courses, which brought the patient a long-awaited recovery and victory over the disease.
To give you an idea of what methods can be used to combat venous insufficiency 2nd degree, let's talk about them in more detail.
How is CVI (chronic venous insufficiency) treated?
First of all, the patient, in the absence of contraindications, is prescribed to wear compression hosiery, which improves local blood flow in the lower extremities. In addition, the doctor prescribes ointments and gels containing heparin. The doctor may also recommend taking medications that improve blood counts (for example, reduce blood clotting).
However, in some cases more radical methods of treating CVI are required, these include:
. Sclerotherapy. This procedure is a medical procedure during which a sclerosant is injected into the affected vein - a substance that causes local destruction of the walls of the vessel and narrowing of the lumen inside it. The vein literally “sticks together”, while being completely excluded from the bloodstream. The blood is distributed to other healthy vessels of the superficial veins. A similar method is used in the case of varicose veins of relatively small diameter. In some situations, a whole course of sclerosant injections may be required for the vein to disappear. The advantage of sclerotherapy is its low invasiveness and absence of side effects (this statement is only true if the procedure is carried out correctly) and rapid rehabilitation of the patient. With its help, you can achieve the desired cosmetic effect, as well as improve tissue trophism by tidying up the blood flow in the area of the lower extremities. It should be noted that injections are performed under local anesthesia, which is a clear advantage compared to larger operations that are performed using systemic anesthesia. The patient can leave the hospital on the day of sclerotherapy and then only be observed on an outpatient basis.Laser surgery. Laser radiation is a powerful tool to combat the manifestations of venous insufficiency. At the same time, there are no restrictions on the diameter of blood vessels, as is the case with sclerotherapy. The essence of the method is that the surface of the vessel is irradiated from the inside with a laser, which is administered intravenously using a special device. All manipulations are carried out under the control of an ultrasound machine, so the accuracy of the effect is quite high. The laser acts inside the vessel like a sclerosant, causing destruction and gluing of its walls.
Venectomy or surgical stripping of veins. It involves surgical excision of the affected vessels. The operation is performed under general anesthesia. The doctor makes a couple of tiny incisions on the skin, through which the vessels are removed and the perforating veins on the lower leg are ligated. Such surgical interventions are performed on deep veins that have a large diameter.
Ablation. This procedure involves heating the inner wall of the vein by introducing flexible electrodes located at the end of the catheter into it. Once heated, the vein is destroyed.
Venous bypass. In some cases, the development of CVI involves vein shunting using an artificial connecting vessel (called a conduit). This operation is performed in the most severe cases of venous insufficiency when all of the above methods fail.
In our center you can undergo high-quality vascular diagnostics using duplex scanning, which will help accurately identify problem areas in the veins. Our goal is to treat venous insufficiency using the most gentle methods. If only conservative therapy is sufficient to cure the patient, then we will limit ourselves to it. Otherwise, we will use the entire range of innovative techniques in the field of vascular surgery and perform low-traumatic manipulations aimed at restoring local blood flow and putting in order the trophism in the tissues of the lower extremities. The price of treatment in our medical institution is economically justified and affordable even for people with average income.
Our doors are open to everyone who wants to get rid of varicose veins and related diseases efficiently and quickly. We are ready to help everyone who needs it!
Related materials:Chronic venous insufficiency of the lower extremities is a syndrome caused by impaired blood flow from the leg area. CVI in most cases is caused by the gravitational factor, which has a significant effect on blood flow in the human body. Chronic venous insufficiency of the lower extremities is rightfully considered a disease of civilization as a “payback” for walking upright. According to statistics, more than 35% of the world's population is susceptible to the development of certain vascular pathologies.
CVI is diagnosed mainly in socially active people aged 22 to 55 years, who, due to their activities, spend a long time in a standing or sitting position. This places undue stress on the lower extremities and ultimately leads to venous insufficiency.

The concept of chronic venous insufficiency of the lower extremities (CVI) implies a whole set of disorders and includes the following pathologies:
- Phlebeurysm.
- Postthrombotic pathology.
- Congenital and acquired vascular pathologies are also possible.
With CVI, there is a significant increase in pressure in the area of veins and vessels, increased permeability and swelling of the venous walls. As a result, venous insufficiency can lead to disruption of tissue trophism, which provokes the development of ulcers and eczema in the lower extremities, which are difficult to treat.

Chronic venous insufficiency of grade 1 or 2 develops under the influence of the following factors:
- Hereditary predisposition to the development of venous insufficiency.
- Lack of physical activity.
- Excess weight.
- Exposure to systematic intense physical strain, which is accompanied by lifting heavy objects.
- Prolonged stay in hot climates.
- Tendency to defecation disorders.
- The period of pregnancy (especially the second or third).
- In general, representatives of the fair sex are more predisposed to the development of CVI.
The main factor that provokes venous insufficiency in the lower extremities at the 2nd or 1st stage of development is a disruption of the normal functioning of the venous-muscular pump.
A person is predominantly in an upright position, which greatly complicates the movement of blood upward to the heart area. Stagnation of blood leads to a gradual stretching of veins and vessels, and the functional ability of the venous valves is impaired.
If there are risk factors, a person may develop grade 1 chronic venous insufficiency, which will gradually progress in the absence of proper treatment.
Manifestations of pathology

Chronic venous insufficiency of the lower extremities has a number of characteristic symptoms that appear depending on the degree of venous damage.
CVI of the lower extremities can significantly impair the quality of life of men and women at any phase of its development. The danger is that stage 1 chronic venous insufficiency may not manifest itself for a long time, while the pathology itself slowly progresses. Most patients seek help already with stage 2 CVI or, worse, with stage 3 CVI.
Zero and first stage

First of all, doctors distinguish 0 degree CVI. In this case, a small vascular pattern is formed on the surface of the skin, which is not accompanied by swelling or the development of pain. Such a symptom is more of a cosmetic defect for the patient, but not a dangerous symptom. You can remove the vascular pattern with a laser, but the disease itself may continue to progress.
Grade 1 venous insufficiency in the lower extremities will manifest itself as follows:
- Development of moderate pain in the legs.
- Complaints of heaviness in the legs of varying intensity, tired leg syndrome.
- CVI degree 1 is accompanied by the formation of edema that occurs after a hard day of work and goes away on its own after rest. In most cases, the ankles swell, but the toes remain normal.
- With CVI at this stage, a small vascular pattern may be visible in the form of protruding purple-blue “stars” and “webs” on the surface of the skin.
The doctor will prescribe a comprehensive examination and, based on its results, recommend appropriate therapy. It is easiest to stop the progression of stage 1 CVI, so you should not leave the first alarm bells without proper attention.
Treatment

The main goals of therapy are:
- Normalize the functioning of the lymphatic and venous system.
- Prescribe preventive treatment to stop further progression of the disease.
To eliminate cosmetic imperfections at stages 0 and 1 in the form of the formation of a vascular pattern, sclerotherapy is most often used. A special substance, a sclerosant, is injected into the vein area, which glues the lesion from the inside and blood continues to flow freely through healthy vessels and veins. For the purpose of prevention, medications can be prescribed that strengthen the walls of blood vessels and prevent the development of trophic disorders. The following groups of medications are most often used in treatment regimens:
- Medicines based on diosmin: Phlebodia, Detralex.
- Troxerutin-based products: Troxevasin.
- Products containing horse chestnut extract: Aescusan, Venoton.
Such medicines can be used for a long time.
If there are no complications in the form of thrombophlebitis, the use of external heparin-based preparations is not advisable. The exact regimen and duration of treatment can only be determined by a phlebologist, taking into account the degree of development of the disease, its manifestations and the characteristics of the patient’s body.
Second stage

In the absence of adequate treatment and preventive measures, chronic venous insufficiency continues to progress and reaches the 2nd stage of development. With CVI of the 2nd degree, the following symptoms may occur, indicating the development of the problem:
- The pain in the legs becomes more intense. The patient may describe the feeling of pain as “bursting”, accompanied by a burning sensation.
- The 2nd degree of damage is characterized by the development of cramps in the calf muscles, which bother the patient mainly at night.
- When the limbs are affected at stage 2, swelling becomes more persistent and can occur both in the evening and during the day.
- The 2nd degree of development of venous disorders is characterized by changes in the skin of the affected limb: they may acquire a pale color and become cold to the touch. In some cases, grade 2 CVI is accompanied by hyperpigmentation in the form of brown spots in the lower leg area.
With CVI at stage 2, the development of lipodermatosclerosis may be observed, which is accompanied by inflammation of the skin and the development of pain.
The skin takes on a red tint, and a few eczemas may form. A similar reaction of the body with stage 2 disease development indicates excessive thinning of the skin in the area of dilated veins. In addition, the patient experiences severe itching at the site of the lesion, and the skin may become spotty.
Benefits of Physiotherapy

Physiotherapeutic treatment methods can be used at any stage of development of venous insufficiency in the case of objective indications and on the recommendation of a doctor. Positive therapeutic effects have:
- Involvement of diadynamic currents.
- Electrophoresis therapy.
- Using a laser.
- Magnetic fields.
If conservative methods of therapy have had a positive effect, in the future the patient will be advised to adjust his usual lifestyle:
- Review your diet.
- Use compression stockings or elastic bandages, including before playing sports.
- Preventive treatment using certain groups of medications recommended by the doctor.
How to use elastic compression correctly

It is important to know how to use elastic bandages correctly. The bandage should be applied to the affected limb immediately after waking up, when the patient has not yet risen from bed. The bandage should be applied from bottom to top, while grasping the foot. Each subsequent turn of the bandage around the foot should overlap the previous one by 2/3, but the compression should not be applied too tightly. If the patient feels severe discomfort, numbness in the toes or pain, then it is necessary to bandage the leg.
If necessary, it is allowed to apply heparin ointment or troxerutin gel under the bandage to enhance the positive therapeutic effect.
The selection of suitable compression stockings should also be entrusted to a doctor. Elastic stockings, tights and knee socks are distinguished by the degree of compression. For prevention, lighter compression is used; in severe cases, the degree of compression of the limb should be maximum.
Third stage

Chronic venous insufficiency of the 3rd degree is accompanied by the development of:
- Trophic disorders: ulcerative skin lesions.
- Bleeding.
- Thrombosis affecting deep veins.
- Thrombophlebitis.
The development of ulcerative skin lesions during CVI at stage 3 of the disease occurs as follows:
- At the initial stage, the skin with venous insufficiency turns brown.
- Next, a small dense formation forms in the center of the colored area; the skin in this place may shine, as if it were covered with a layer of paraffin.
- This condition can persist for a long time; in the future, even the smallest injury leads to the formation of an open wound and the development of ulcerative skin lesions.
In the event that there is no proper therapy, with the 3rd degree of damage there is a high probability of the addition of an infectious pathogen, which threatens the development of serious complications.
Therapy

With the development of trophic disorders, treatment of the disease becomes much more complicated. In this case, it is necessary to involve a whole range of measures: the use of medications for internal use and external application, elements of physiotherapy. The most commonly used external treatments are:
- Antiseptic preparations for wound treatment.
- Use of enzyme drugs.
- Drugs that accelerate tissue regeneration.
- If necessary, antibacterial agents can be used.
In severe cases, surgery may be required, which involves removing dead skin to prevent the necrotic process from spreading. After treating the wound with a solution of chlorhexidine, peroxide and saline, the patient should apply Levomekol, Levosin ointment or another drug recommended by the doctor.
Treatment of the affected surface should be carried out regularly and the patient will need to put in a lot of effort so that the wound gradually begins to heal.
In what cases may surgical intervention be required?

Treatment with radical methods may be required in cases where conservative therapy does not have the desired effect and the disease continues to progress. Indications for surgical intervention are:
- Development of complications in the form of thrombosis, thrombophlebitis, bleeding.
- Trophic ulcers that do not heal over a long period of time.
- Pronounced cosmetic imperfections such as the formation of voluminous nodes on the surface of the skin and a pronounced vascular pattern.
Radical treatment of venous insufficiency involves removal of the affected area of the vein. In severe cases of pathology, removal of the entire vein may be indicated. The selection of the appropriate treatment method is carried out by the doctor, taking into account the results of the examination and examination.
During the recovery period, it is necessary to strictly follow all the doctor’s recommendations in order to speed up the healing process and minimize the risk of developing possible postoperative complications. In order to prevent the development of stagnation, the patient is recommended to start moving on the 2nd day after the procedure. During the recovery period, it is necessary to use compression hosiery, heparin-based topical medications and other groups of medications recommended by the doctor.
Basic diagnostic methods

The symptoms of CVI can be similar to the symptoms of many other diseases. Only an experienced specialist can make an accurate diagnosis after a comprehensive examination. In most cases, the patient is recommended to undergo the following diagnostic methods:
- Carrying out a general blood test to determine the total number of red blood cells and hemoglobin level. This study allows you to analyze the viscosity and degree of blood clotting. Platelets indicate possible deviations in the blood coagulation system, the presence of leukocytes indicates the development of an inflammatory process.
- Biochemical analysis of urine and blood.
- A highly specialized diagnostic method is an ultrasound examination of the veins and vessels of the legs. According to the study, it is possible to identify the exact localization of the development of the inflammatory process, the presence of varicose veins, varicose veins, blood clots. Ultrasound examination is mandatory for even the most minor manifestations of CVI.
If the results of ultrasound examination are insufficiently informative, the patient is additionally prescribed phlebography. In this case, the doctor injects a special contrast agent into the area of the affected limb and can assess the general condition of the venous system.
What complications may arise?

Untimely or poor-quality treatment of venous insufficiency can lead to the development of the following complications:
- Deep vein thrombosis, which is accompanied by the formation of thrombotic masses that can completely block the lumen of the vessel.
- Thrombophlebitis, in which the inflammatory process affects the walls of blood vessels. This complication is often concomitant with thrombosis.
- Disturbances in the normal functioning of the lymphatic system. At the same time, swelling bothers the patient regularly and no longer goes away on its own. This is due to a disruption in the flow of lymph in the area of the affected leg.
The danger lies in the fact that even a minor injury can lead to the development of heavy bleeding. In this case, it is recommended to bandage the affected limb as soon as possible with a tourniquet slightly above the site of injury and take the patient to the hospital. The development of bleeding from the affected, dilated vein can pose a threat to the patient’s life, so in this case you should not hesitate in any case.
Preventive actions

The doctor can give the patient recommendations regarding the primary prevention of venous insufficiency and advise eliminating possible risk factors. The development of chronic venous insufficiency is easier to prevent than to cure. Therefore, patients at risk are advised to take into account the following recommendations regarding the prevention of the disease:
- It is recommended to give up bad habits: drinking alcohol, smoking. Under the influence of harmful substances, the vascular wall becomes thinner, veins and vessels gradually stretch.
- Moderate physical activity helps prevent the development of stagnation. Therefore, daily walking, visiting the pool, yoga and gymnastics will help prevent the premature development of problems with veins and blood vessels. When playing sports, it is recommended to use elastic bandages and compression stockings.
- Women expecting a baby and prone to developing venous insufficiency are recommended to systematically undergo ultrasound examination of the vessels of the legs.
- Overweight patients are recommended to normalize their weight.
- It is also recommended to review the diet and introduce fresh fruits and vegetables, dried fruits, dairy products, and herbs.
- During rest, it is recommended to keep the limbs in an elevated position and place a splint or small pillow under them.
- It is recommended to give preference to comfortable, non-tightening shoes and clothing. Women are advised to avoid frequent wearing of high heels.
For the purpose of prevention, patients may be recommended to take regular courses of medications and a group of phlebotonics. Some preventive therapy regimens involve internal administration of the drug Phlebodia and external application of the drug Troxevasin in the form of a gel.
website - a medical portal about the heart and blood vessels. Here you will find information about the causes, clinical manifestations, diagnosis, traditional and folk methods of treating cardiac diseases in adults and children. And also about how to keep the heart healthy and blood vessels clean until old age.
Do not use the information posted on the site without first consulting your doctor!
The authors of the site are practicing medical specialists. Each article is a concentrate of their personal experience and knowledge, honed over years of study at the university, received from colleagues and in the process of postgraduate training. They not only share unique information in articles, but also conduct a virtual consultation - answer questions you ask in the comments, give recommendations, help you understand the results of examinations and prescriptions.
All topics, even those that are very difficult to understand, are presented in simple, understandable language and are intended for readers without medical training. For your convenience, all topics are divided into sections.
Arrhythmia
According to the World Health Organization, arrhythmias, irregular heartbeats, affect more than 40% of people over 50 years of age. However, they are not the only ones. This insidious disease is detected even in children and often in the first or second year of life. Why is he cunning? And because it sometimes disguises pathologies of other vital organs as heart disease. Another unpleasant feature of arrhythmia is the secrecy of its course: until the disease goes too far, you may not be aware of it...
- how to detect arrhythmia at an early stage;
- which forms are the most dangerous and why;
- when is enough for the patient, and in what cases is surgery indispensable;
- how and how long do they live with arrhythmia;
- which attacks of arrhythmia require an immediate call to the ambulance, and for which it is enough to take a sedative pill.
And also everything about the symptoms, prevention, diagnosis and treatment of various types of arrhythmias.
Atherosclerosis
It is written in all newspapers that the main role in the development of atherosclerosis is played by excess cholesterol in food, but why then in families where everyone eats the same, often only one person gets sick? Atherosclerosis has been known for more than a century, but much of its nature remains unsolved. Is this a reason to despair? Of course not! The site’s specialists tell you what successes modern medicine has achieved in the fight against this disease, how to prevent it and how to effectively treat it.
- why margarine is more harmful than butter for people with vascular damage;
- and why it is dangerous;
- why cholesterol-free diets don't help;
- what will patients with;
- how to avoid and maintain mental clarity into old age.
Heart diseases
In addition to angina pectoris, hypertension, myocardial infarction and congenital heart defects, there are many other cardiac ailments that many have never heard of. Did you know, for example, that it is not only a planet, but also a diagnosis? Or that a tumor can grow in the heart muscle? The section of the same name talks about these and other heart diseases in adults and children.
- and how to provide emergency care to a patient in this condition;
- what to do and what to do so that the first does not turn into the second;
- why the heart of alcoholics increases in size;
- Why is mitral valve prolapse dangerous?
- What symptoms can you use to suspect that you and your child have heart disease?
- which cardiac diseases are more threatening to women and which ones to men.

Vascular diseases
Vessels permeate the entire human body, so the symptoms of their damage are very, very diverse. Many vascular diseases do not bother the patient much at first, but lead to serious complications, disability and even death. Can a person without medical education identify vascular pathology in himself? Of course, yes, if he knows their clinical manifestations, which this section will talk about.
In addition, here is the information:
- about medications and folk remedies for the treatment of blood vessels;
- about which doctor to contact if you suspect vascular problems;
- what vascular pathologies are deadly?
- what causes veins to swell;
- How to keep your veins and arteries healthy for life.
Varicose veins
Varicose veins (varicose veins) are a disease in which the lumens of some veins (legs, esophagus, rectum, etc.) become too wide, which leads to impaired blood flow in the affected organ or part of the body. In advanced cases, this disease is cured with great difficulty, but at the first stage it can be curbed. How to do this, read in the section “Varicose veins”.
 Click on photo to enlarge
Click on photo to enlarge You will also learn from it:
- what ointments exist for the treatment of varicose veins and which one is more effective;
- why doctors prohibit some patients with varicose veins of the lower extremities from running;
- and who it threatens;
- how to strengthen veins with folk remedies;
- how to avoid blood clots in affected veins.
Pressure
- such a common illness that many consider it... a normal condition. Hence the statistics: only 9% of people suffering from high blood pressure keep it under control. And 20% of hypertensive patients even consider themselves healthy, since their disease is asymptomatic. But the risk of getting a heart attack or stroke is no less! Although it is less dangerous than high, it also causes a lot of problems and threatens with serious complications.

In addition, you will learn:
- how to “deceive” heredity if both parents suffered from hypertension;
- how to help yourself and your loved ones during a hypertensive crisis;
- why blood pressure increases at a young age;
- how to keep your blood pressure under control without medications by eating herbs and certain foods.
Diagnostics
The section devoted to the diagnosis of heart and vascular diseases contains articles about the types of examinations that cardiac patients undergo. And also about indications and contraindications to them, interpretation of results, effectiveness and procedures.
You will also find answers to questions here:
- what types of diagnostic tests even healthy people should undergo;
- why is angiography prescribed for those who have suffered a myocardial infarction and stroke;

Stroke
Stroke (acute cerebrovascular accident) is consistently among the ten most dangerous diseases. People at greatest risk of developing it are people over 55 years of age, hypertensive patients, smokers and those who suffer from depression. It turns out that optimism and good nature reduce the risk of strokes by almost 2 times! But there are other factors that effectively help avoid it.
The section dedicated to strokes talks about the causes, types, symptoms and treatment of this insidious disease. And also about rehabilitation measures that help restore lost functions to those who have suffered from it.

In addition, here you will learn:
- about the differences in clinical manifestations of strokes in men and women;
- about what a pre-stroke condition is;
- about folk remedies for treating the consequences of strokes;
- about modern methods of rapid recovery after a stroke.
Heart attack
Myocardial infarction is considered to be a disease of older men. But the greatest danger it poses is not for them, but for people of working age and women over 75 years of age. It is in these groups that mortality rates are highest. However, no one should relax: today heart attacks overtake even the young, athletic and healthy. More precisely, underexamined.
In the “Heart Attack” section, experts talk about everything that is important to know for everyone who wants to avoid this disease. And those who have already suffered a myocardial infarction will find here many useful tips on treatment and rehabilitation.

- about what diseases a heart attack is sometimes disguised as;
- how to provide emergency care for acute pain in the heart area;
- about differences in the clinical picture and course of myocardial infarction in men and women;
- about an anti-heart attack diet and a heart-safe lifestyle;
- about why a person suffering from a heart attack must be taken to a doctor within 90 minutes.
Pulse abnormalities
When we talk about pulse abnormalities, we usually mean its frequency. However, the doctor evaluates not only the speed of the patient’s heartbeat, but also other indicators of the pulse wave: rhythm, filling, tension, shape... The Roman surgeon Galen once described as many as 27 of its characteristics!

Changes in individual pulse parameters reflect the state of not only the heart and blood vessels, but also other body systems, for example, the endocrine one. Want to know more about this? Read the materials in the section.
Here you will find answers to questions:
- why, if you complain of pulse irregularities, you may be referred for a thyroid examination;
- whether a slow heart rate (bradycardia) can cause cardiac arrest;
- what does it mean and why is it dangerous;
- how heart rate and the rate of fat burning when losing weight are interconnected.
Operations
Many heart and vascular diseases, which 20–30 years ago doomed people to lifelong disability, can now be successfully cured. Typically surgically. Modern cardiac surgery saves even those who until recently were given no chance to live. And most operations are now performed through tiny punctures, rather than incisions, as before. This not only gives a high cosmetic effect, but is also much easier to tolerate. It also reduces the postoperative rehabilitation time by several times.
In the “Operations” section you will find materials about surgical methods for treating varicose veins, vascular bypass surgery, installation of intravascular stents, heart valve replacement, and much more.
You will also learn:
- which technique does not leave scars;
- how operations on the heart and blood vessels affect the patient’s quality of life;
- what are the differences between operations and vessels;
- for what diseases is it performed and what is the duration of a healthy life after it;
- What is better for heart disease - to be treated with pills and injections or to undergo surgery.

Rest
“Rest” includes materials that do not correspond to the topics of other sections of the site. Here you can find information about rare cardiac diseases, myths, misconceptions and interesting facts regarding heart health, unclear symptoms and their significance, the achievements of modern cardiology and much more.
- about providing first aid to yourself and others in various emergency conditions;
- about the child;
- about acute bleeding and methods to stop it;
- o and eating habits;
- about folk methods of strengthening and healing the cardiovascular system.

Drugs
“Drugs” is perhaps the most important section of the site. After all, the most valuable information about a disease is how to treat it. We do not provide here magical recipes for curing serious illnesses with one tablet; we honestly and truthfully tell everything about the drugs as they are. What are they good for and what are they bad for, for whom are they indicated and contraindicated, how do they differ from analogues and how do they affect the body. These are not calls for self-medication, this is necessary so that you have good command of the “weapons” with which you have to fight the disease.

Here you will find:
- reviews and comparisons of drug groups;
- information about what can be taken without a doctor’s prescription and what should not be taken under any circumstances;
- a list of reasons for choosing one or another means;
- information about cheap analogues of expensive imported drugs;
- data on the side effects of heart drugs that manufacturers are silent about.
And many, many more important, useful and valuable things that will make you healthier, stronger and happier!
May your heart and blood vessels always be healthy!





